The Retroviruses
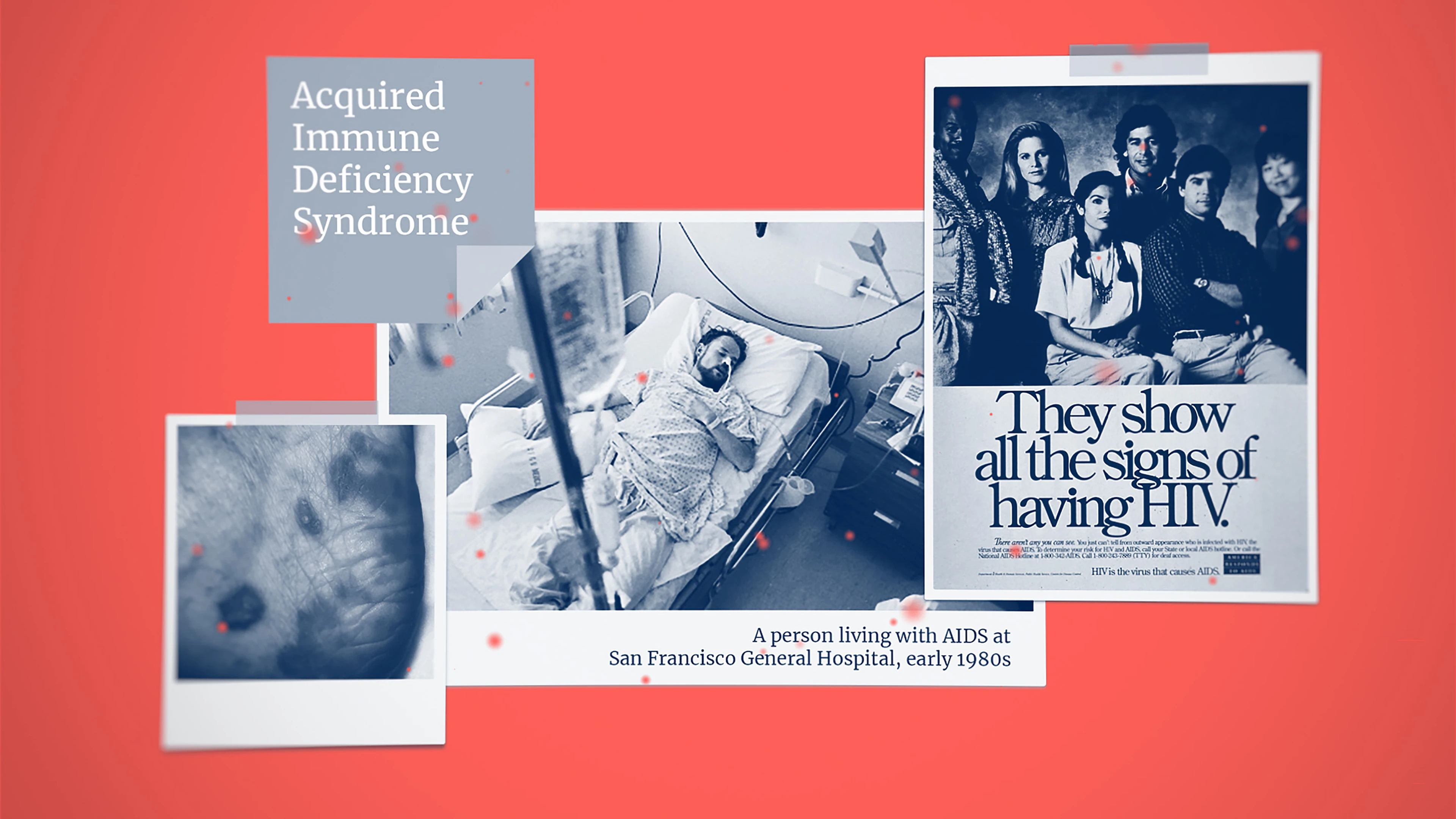
According to a New York Times article in the summer of 1981, dozens of young and otherwise healthy men appeared rather suddenly to be falling victim to a usually rare type of cancer.
The disease began with one or more violet-coloured spots or blotches that could crop up anywhere on the body and could easily be mistaken for bruises. Unlike bruises, however, the purple-blue blotches persisted for many weeks, sometimes developing into lumps and turning brown. The strange disease appeared to progress rapidly in these young victims, next causing painfully swollen lymph glands and then spreading swiftly—and fatally—throughout the whole body.
These were the first reports of Acquired Immune Deficiency Syndrome, an incurable deadly condition which was recognised as a new disease that same year—1981—and which is now known to most people as AIDS. In a letter alerting other doctors to the situation and asking them to keep an eye out for similar cases, Dr. Alvin E. Friedman-Kien of New York University Medical Center described the outbreak as “rather devastating”.
He could not have known then how accurate a description this would be.
Within a couple of years, the cause of AIDS was identified as a virus that had almost certainly jumped from chimpanzees into humans at least several decades earlier somewhere in Central Africa. The virus—now known as Human Immunodeficiency Virus, or HIV—has since infected an estimated 85 million people all across the world, killing more than 40 million of them. The HIV/AIDS pandemic’s most devastating and disproportionate impact has been in sub-Saharan Africa, where an estimated 25.6 million people were living with HIV as of 2022—accounting for more than two-thirds of the global total. There's little doubt, then, that HIV is by far the most notorious killer in its viral family—the Retrovirus Family, one of The Viral Most Wanted.
One Big Close-Knit Family?
It’s a big family, yes, but its members are not particularly close. The Retrovirus family is made up of three distinct subgroups—Oncoretroviruses, Lentiviruses and Spumaviruses—each of which has a different impact or disease-causing capability in different groups of animals or humans. The number of Retroviruses that cause human disease is relatively small, with just six known to date. Four of these—known as Human T-Lymphotropic Virus types 1, 2,3 and 4—belong to the Oncoretrovirus subgroup because they cause cancer in people. The other two—Human Immunodeficiency Virus type 1 and Human Immunodeficiency Virus type 2—belong to the Lentivirus subgroup.
Prime Suspects
By far the most infamous and pernicious member of the Retrovirus family is the Human Immunodeficiency Virus—the virus that causes the deadly human disease AIDS. The ongoing worldwide AIDS pandemic that has already killed more than 40 million people is caused by the Retrovirus HIV-1 Group M.
Besides HIV, there are several other retroviruses that can cause human illness. One is Human T-Lymphotropic Virus type 1 and another is Human T-Lymphotropic Virus type 2. These viruses can cause a type of cancer called adult T-cell leukaemia/lymphoma, or ATL, as well as a progressive condition of the nervous system known as HTLV-1-Associated Myelopathy or Tropical Spastic Paraparesis.
Nicknames and Aliases
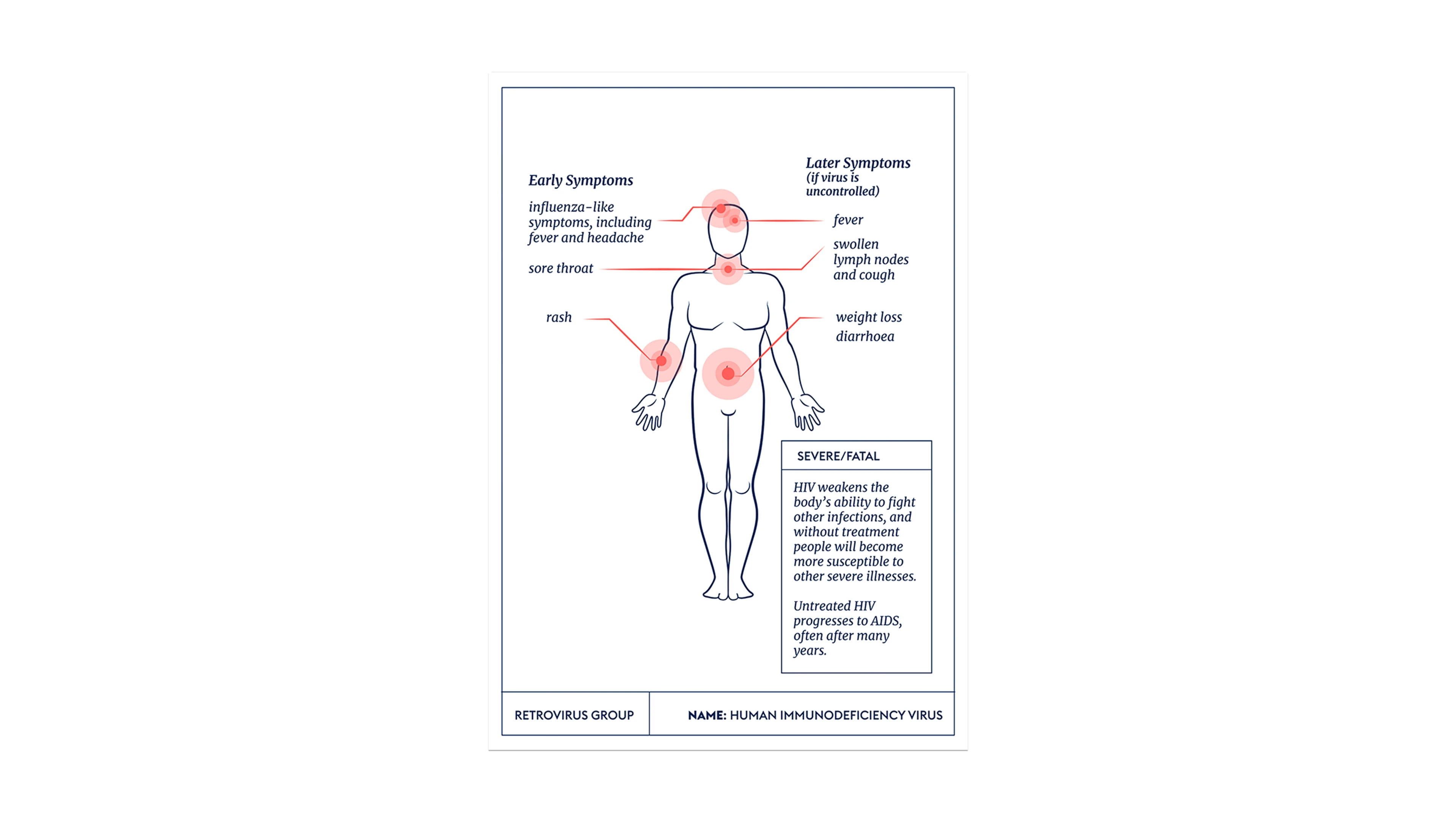
The Human Immunodeficiency Virus is most commonly referred to as HIV, but also often known as the virus that causes AIDS—itself an acronym for Acquired Immune Deficiency Syndrome.
The Human T-Lymphotropic Viruses type 1 and type 2 are also known by the acronyms HTLV-1 and HTLV-2, or as Human T-cell Leukaemia Virus type 1 and type 2.
Distinguishing Features
Retrovirus particles, or virions, are small spheres of around 80 to 100 nanometres in diameter and have a lipid envelope, or cloak. Protrusions made of glycoproteins stick out from the virion’s surface and tend to be around eight nanometers long. An inner protein core contains the viral genome and the enzymes the virus needs to be able to replicate.
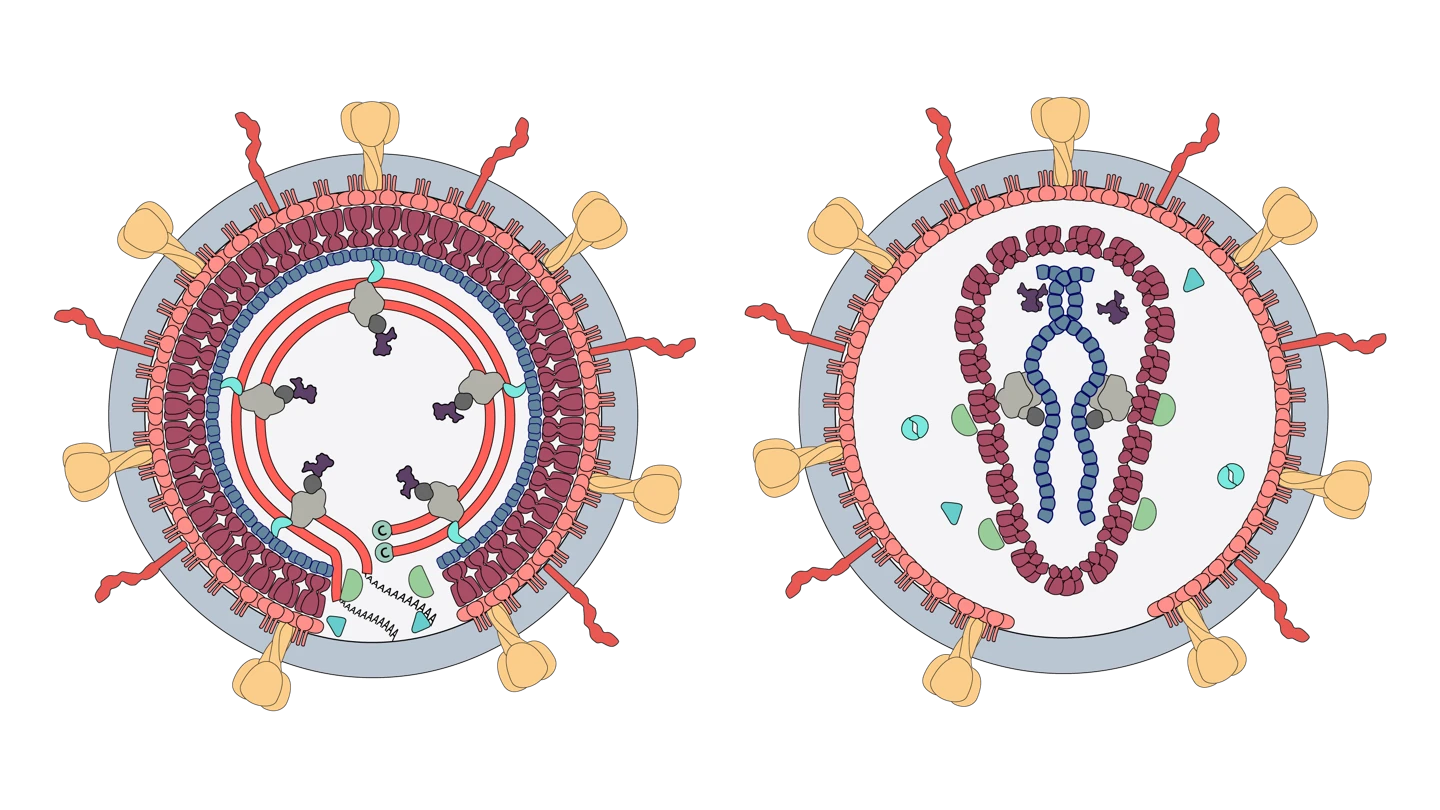
Source: Viral Zone by SwissBioPics
Modus Operandi
When a member of the Retrovirus family enters a host cell it uses a special enzyme called reverse transcriptase to create DNA using the information in its RNA genome. This is the opposite of what viruses usually do, which is why these viruses have earned the name “retro”, which means backwards. It then inserts that DNA copy into the host cells it has invaded. The cells then produce more retroviruses, which in turn infect other cells.
When the HIV Retrovirus gets inside the human body, it focuses its attack on the immune system—specifically on a type of white blood cell in the immune system called CD4 cells. HIV gets into the CD4 cells and makes copies of itself—or replicates—inside them before killing them. While the new HIV copies find other CD4 cells to do the same thing, the body’s immune system tries to fight back and control the HIV by making more CD4 cells. Unfortunately, in almost all cases, the immune system is running a losing race and can’t make new CD4 cells fast enough. This is when the HIV takes over and starts to destroy the immune system.
Accomplices
Retroviruses use no accomplices to spread between people. They are transmitted directly through contact with various bodily fluids of an infected person, including blood, semen and breast milk. This means that the main accomplice of HIV is human behaviour. People who have unprotected sex with, or share needles with, someone who is HIV positive are at very high risk of also becoming infected. Mothers who are HIV positive can pass HIV on to their newborn babies during pregnancy and childbirth or via breastfeeding.
The other two retroviruses that cause human disease, HTLV-1 and HTLV-2, are also transmitted via sexual contact, exposure to infected blood or tissue, or during pregnancy or childbirth from an infected mother to her baby.

Common Victims
Any person of any age, gender or ethnicity can fall victim to infection with HIV. It is a virus that exploits certain kinds of behaviours to spread, rather than targeting particular kinds of people. Because it is transmitted via blood and semen, its most common victims are people who share needles to inject drugs or who engage in high-risk sexual behaviours, including unprotected sex with multiple partners, any one of whom may already be infected with the virus and not yet know it.
Victims of infection with the HTLV-1 retrovirus can also be anyone of any age, but the virus is endemic in, and therefore most prevalent in, the Caribbean, South America, Romania, Iran, much of Africa, Japan, Melanesia and indigenous people in Australia.
HTLV-2, which is rarer than HTLV-1, is most frequently found in people from West and Central Africa and in indigenous Americans.
Infamous Outbreaks
By far the largest and longest-running human Retrovirus outbreak is the HIV/AIDS pandemic. Disease trackers’ estimates are that since the beginning of the global outbreak, some 85.6 million people have been infected with HIV, and about 40.4 million of them have died. The World Health Organization (WHO) estimates that some 39 million people worldwide are living with HIV.
Africa is by far the worst affected region, with more than two-thirds of all those infected with the virus living there. At the end of 2022, one in every 25 adults in the WHO’s Africa region—or 3.2 percent of the population—was HIV positive.
According to disease estimates from the WHO, between five million and 10 million people around the world are infected with HTLV-1, although experts say the true number could also be higher due to a lack of reliable data and reporting.
Source: IHME, Global Burden of Disease (2019)
Common Harms
Human Immunodeficiency Virus damages the cells in the human immune system and weakens its victims’ ability to fight off everyday infections and disease. Most people suffer a short flu-like illness around two to six weeks after becoming infected with HIV, and these symptoms might continue for a week or two. After the flu-like symptoms fade, HIV might not cause any significant symptoms at all for many months or even years—but during this time the virus is silently and persistently infecting and damaging the cells of the immune system.
Lines of Enquiry
For the HIV Retrovirus, disease detectives have been searching long and hard for many decades to try to design a way to prevent infections and/or cure AIDS. So far, these lines of enquiry have led to some extremely effective medicines that people with HIV can take at regular intervals to keep the virus in check and prevent it from spreading to sexual partners. The medicines—known as anti-retroviral therapy or ART—have also enabled some people with HIV to be able reduce their ‘viral load’ – the amount of virus circulating in their body – to levels where it is undetectable, and therefore untransmissible sexually. ART can also be taken as a prophylactic defence against HIV by people who are at high risk of contracting it.
Unfortunately, access to these life-saving medicines is not universal, leaving many millions of people in poorer countries living with HIV without the drugs that can keep them healthy. By the end of 2022, around 76 percent of people infected with the virus had access to antiretroviral therapy, but 9.2 million HIV-positive people—mostly living in sub-Saharan Africa—did not.
A vast amount of money and scientific expertise over the last 40 years has gone into pursuing lines of enquiry focused specifically on developing an HIV vaccine. Frustratingly, only one of the nine HIV vaccine candidates tested during that time has shown any efficacy; a trial conducted in Thailand and published in 2009 reported a 31 percent reduction in HIV risk among those given an experimental preventative vaccination.
Recently, however, HIV vaccine researchers have been newly invigorated by the advances in vaccinology made during the COVID-19 pandemic.
Seeking to build on the success of messenger RNA vaccines in reducing deaths and disease severity caused by COVID-19, scientists in the U.S. have begun three experimental HIV vaccines based on an mRNA platform.
For the HTLV-1 Retrovirus, there is also currently no vaccine, although experts at the WHO say the development of a vaccine against this Retrovirus is feasible.

Editor's note:
The naming and classification of viruses into various families and sub-families is an ever-evolving and sometimes controversial field of science.
As scientific understanding deepens, viruses currently classified as members of one family may be switched or adopted into another family, or be put into a completely new family of their own.
CEPI’s series on The Viral Most Wanted seeks to reflect the most widespread scientific consensus on viral families and their members, and is cross-referenced with the latest reports by the International Committee on Taxonomy of Viruses (ICTV).










