Middle East Respiratory Syndrome
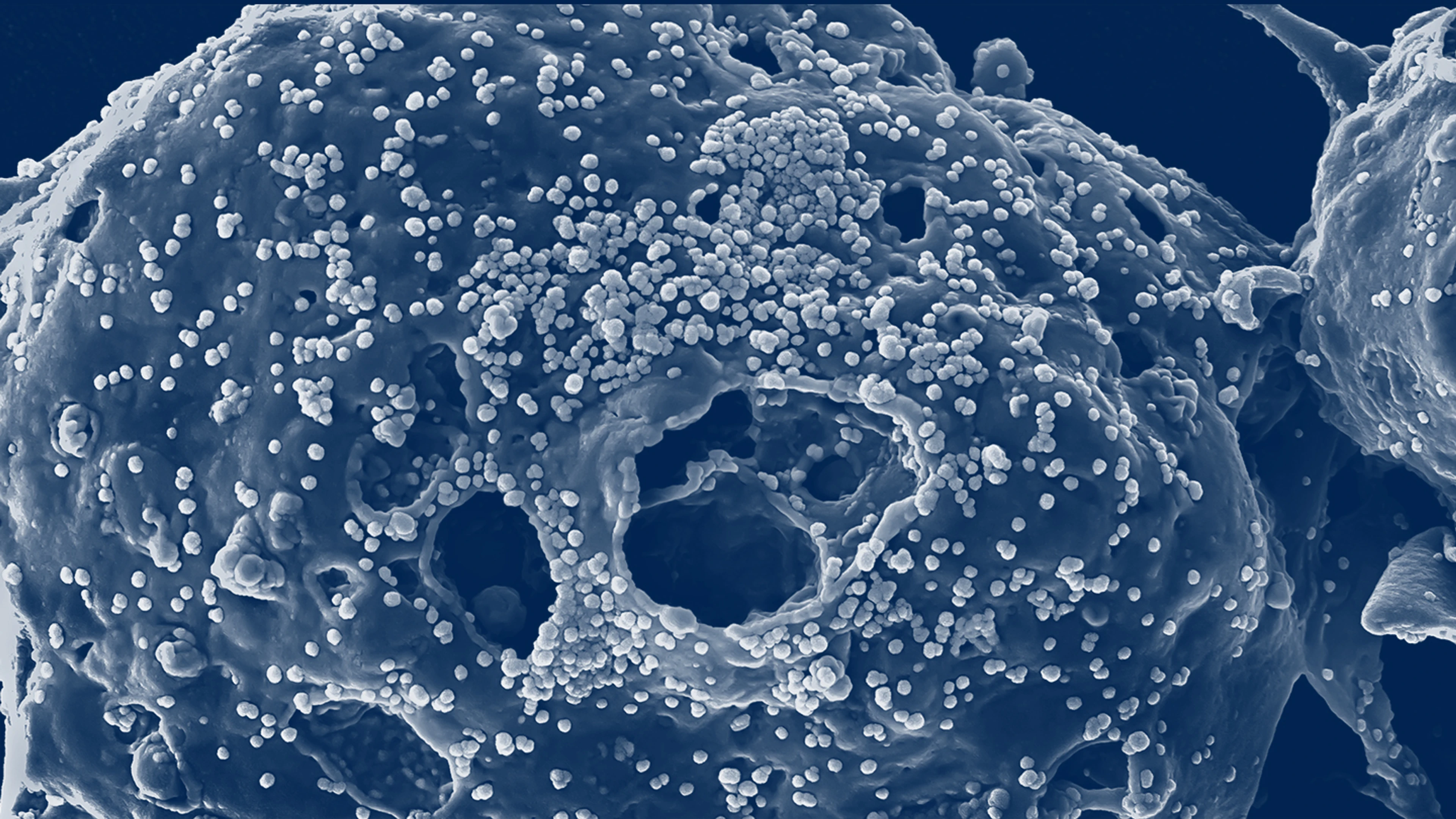
MERS (Middle East Respiratory Syndrome) is a deadly disease caused by MERS-CoV, a coronavirus.
What is MERS?
Middle East Respiratory Syndrome (MERS) is a respiratory illness caused by a coronavirus called Middle East Respiratory Syndrome Coronavirus (MERS-CoV).
This virus belongs to the same family of viruses that causes the common cold, severe acute respiratory syndrome (SARS), and COVID-19.
MERS-CoV is a zoonotic virus which means it spills over from animals, particularly dromedary camels, to humans. Though less common, it can also spread between people via respiratory secretions.
The origins of the virus are not fully understood, but some evidence suggests it may have originated in bats and transmitted to camels sometime in the distant past.

27
Number of countries that have reported cases of MERS-CoV to WHO since 2012
2600+
Number of cases that have been reported since 2012
$10 bn
Estimate cost of 2015 MERS outbreak in South Korea
Where does MERS occur?
The first documented cases of MERS were identified in 2012 in Jordan and Saudi Arabia.
Most cases have been reported from the Arabian Peninsula, with Saudi Arabia reporting about 84% of global total cases. Since 2012, 27 countries have reported cases of MERS to the WHO, of which 12 are in the Eastern Mediterranean WHO region. Sporadic cases still continue to occur on the Arabian peninsula, with a few cases confirmed every year.
In 2015, the Republic of Korea suffered the largest MERS outbreak outside of the Middle East, with 185 laboratory-confirmed cases and 38 deaths reported.
The outbreak was caused by a single case returning from the Arabian Peninsula. Before it was brought under control some two months later, more than 2,700 schools were closed and nearly 17,000 people were quarantined.
Health researchers estimated that the total cost, including losses in retail sales and tourism, approached US $10 billion.

What are the symptoms of MERS infection?
MERS can infect people of any age. However, middle-aged adults are at highest risk of infection.
The disease symptoms vary from no symptoms to mild respiratory illness to severe respiratory disease. Viral infection typically causes respiratory symptoms including cough, shortness of breath and pneumonia.
Other symptoms include fever, headache and diarrhoea. The virus appears to cause more severe disease in older people, people with weakened immune systems and those with chronic diseases, such as renal disease, cancer, chronic lung disease and diabetes.
About 35% of people with confirmed MERS infection have died. However, this may be an overestimate of the true case fatality risk, as mild cases of MERS may be missed by existing surveillance systems.

How is CEPI responding to MERS?
With no vaccines against MERS currently available, CEPI’s aim is to advance MERS vaccine candidates through Phase 2 clinical trials and potentially develop a ready reserve of vaccines that could be used to control regional outbreaks.
CEPI has invested in the development of five MERS vaccine candidates, three of which remain in active development. Two have entered clinical trials.
As a result of the partnerships initiated to advance development of MERS vaccine candidates, CEPI was able to use this knowledge of another coronavirus and act quickly in response to the COVID-19 pandemic in early 2020.
In October 2020, the first WHO International Standard for MERS-CoV antibodies was established by the WHO Expert Committee on Biological Standardization. This standard was developed by the International Vaccine Institute (IVI) and the National Institute for Biological Standards and Control (NIBSC), and was funded and facilitated by CEPI.
Antibody standards act as a comparator to assess the antibody response elicited by candidate vaccines. They are also a valuable tool for wider research on MERS-CoV immunity and can provide immunological data that contributes to the regulatory review of future vaccine candidates.

Latest MERS news

New funding for vaccine to protect against deadly MERS coronavirus

New partnership aims to advance vaccine against MERS coronavirus

Neutralising the threat of MERS

